What social accountability means for frontline health workers--digging into the black box
By Eric Sarriot and Karen Waltensperger, Save the Children USA
Social accountability in health refers to a group of approaches bringing health professionals, providers or managers, together with community members, or clients, in order to improve quality of services by strengthening the accountability of the health system to the population. USAID has supported innovations and social accountability scale up efforts, as illustrated in the picture from SSDI in Malawi. Our professional community is getting a pretty good picture of what works in this approach and little by little, some questions percolate to the surface.
Scale – Professor Jonathan Fox of American University was a speaker at a recent panel organized by the DC Health Systems Board and Save the Children and brought up the topic of scale. He suggested, as did others, that there needs to be a conceptual reboot of transparency, participation, accountability, and most notably, less time spent on ‘scaling up’ and more on ‘taking scale into account’ by promoting accountability at multiple levels to affect sustainable change.
Time – We still live in the world of project cycles. But social systems need to develop ongoing, adaptive processes allowing health systems to address inevitable stumbles, face dysfunctions, and shocks, which may come from staff changes, aftermaths of a strike, election cycles, and many others. Evaluation and learning processes that go beyond pre-post, then-now, and intervention-control proofs-of-concept need to be in place.
Social dynamics – At the micro level, evidence for what happens inside communities, as between communities and health providers, has been growing. And with that a significant question: what could social accountability mean for frontline health workers?
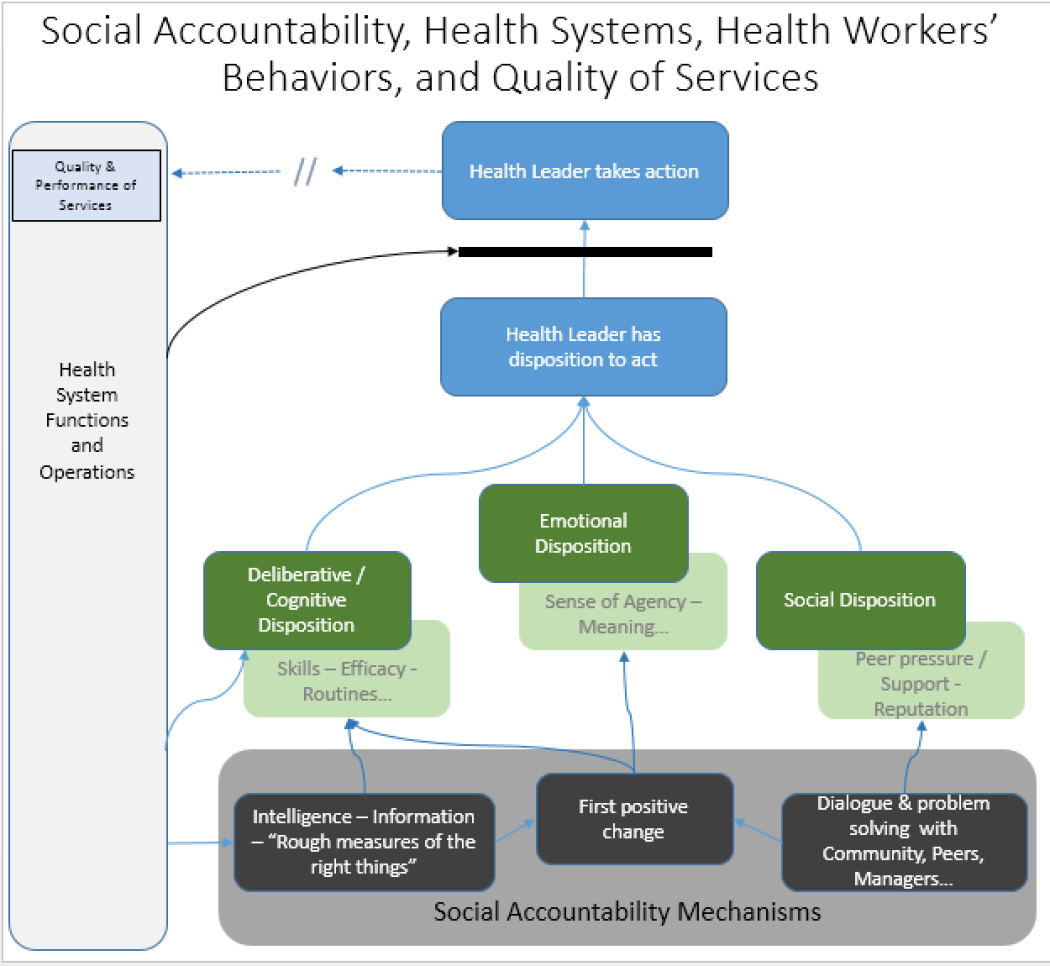
Social accountability and the frontline worker – A frontline health worker can be anyone directly serving clients or communities - a nurse, pharmacist, district supervisor, or other. Accountability mechanisms fundamentally aim to incentivize workers to take [the right] action. In the figure below, taking action is at the very top. Some behavioral theories suggest that a health worker needs to have the “disposition” to act above a certain unknown threshold to take action. The health worker is part of a network and a hierarchy of functions, so right action at one level may affect how this threshold is crossed at another. And when the health system does not provide basic inputs (e.g. drugs), this threshold can be seen as insurmountable. Beyond that, how does disposition to act come along? Disposition accrues from three tracks:
- Deliberative disposition: “I know how to do this; this is what I’m trained for; this will lead to positive outcomes for my patients / my internal clients.”
- Emotional disposition: sense of pride, agency, ownership, meaning, perhaps even fear or shame.
- Social disposition: expectations we attach to social encounters, be they with supervisors, colleagues, clients, or community groups and leaders.
‘Normal’ health systems functions are already affecting these three paths: we train, disseminate information, certify, and supervise to reinforce deliberative factors. We speak about ‘supportive’ supervision, to influence both emotional and social factors. We create quality teams--probably as much a social disposition driver, as a way to cognitively review data. But gaps in performance and quality remain frequent. And accountability mechanisms are proposed to palliate some of these gaps, building micro (health workers’) positive behaviors and accruing system changes through these same pathways:
- Deliberative and cognitive factors are addressed through problem definition (“How do you understand this problem?”), followed by the recourse to measurement and assessments;
- Initiatives often start with our proverbial ‘low hanging fruits’ [cringe] – the reason for this might lie with the emotional value of achieving some success; and
- Finally, accountability may be one of the ways through which we perhaps unwittingly create different types of social capital within groups (providers, communities) and between these groups.
Questions need to be explored in all three pathways. How do we balance objective measures of service performance with subjective assessments and self-assessments? How much ‘demotivation’ is rooted in fatigue from business as usual, and how can initial positive changes snowball to larger ones? How do we address power and conflict as we take scale into consideration? Etc. If we believe in this accountability business, we will need to advance on our macro (scale and time) questions, while continuing to build on experience and evidence about community capacity and social capital. We may also have to dig a bit more into the black box of how health workers’ disposition to act is supported and strengthened by more than cognitive processes. Donor investments for research, and implementation will be needed to help us move frontline health workers into the sort of functional and learning system, which transparency, participation, and accountability can help advance.
