For Health Workers, Responding to Outbreaks Isn’t New
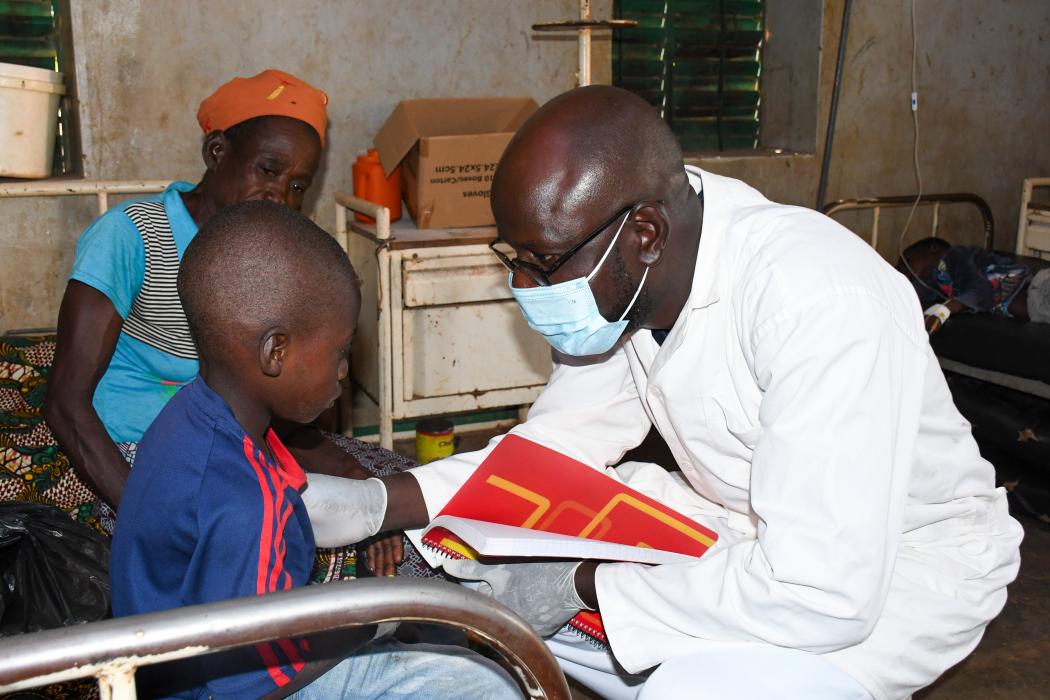
Roger Zingue (right) is the nurse in charge of the Primary Health Care Center at the Bolember health facility in rural Burkina Faso. Photo by Souleymane Zare for Jhpiego.
If we want to place health back on the high-level political agenda and strengthen global health security, we need to listen to health workers at this week’s UN High-Level Meetings on Health.
Primary health care workers are often the first and main point of contact for health services for most people around the world. That means health workers often know about a community outbreak before anyone else, and are responsible for putting measures in place to decrease the spread of the disease. Because global health security has always been part of primary health care.
Health workers, like Roger Zingue, the state nurse in charge of a Primary Health Care Center at the Bolember health facility in rural Burkina Faso, are trained on how to respond to outbreaks. Roger has more than 17 years of experience, including working as head nurse in the country’s southwest region. He’s responded to various infectious diseases and outbreaks, well before COVID-19 was a disease we all knew, and because of that, he knew how to respond in early 2020 when the pandemic hit.
Health workers like Roger Zingue are trained on how to respond to outbreaks.
To achieve universal health coverage, we must acknowledge the connection between primary health care and global health security. That connection is health workers. They provide a range of health services, identify and respond to outbreaks, and engage their communities in health care by addressing misconceptions and promoting healthy behaviors.
This week, during the United Nations (UN) General Assembly—and the UN High-Level Meetings on Pandemic Prevention, Preparedness and Response and on Universal Health Coverage—hear from Roger himself, about how he keeps his community safe from pandemic threats.
Q: Roger, you’ve responded to many outbreaks in your community. Can you share your approach and how you prepare your community members when you know they are at risk of an infectious disease?
January is the start of meningitis season in my region of Burkina Faso. But the community health workers we work with are always ready. They're our strongest connection to the community and they’ve been trained to identify the symptoms. For example, this past meningitis season, a community health worker identified someone with symptoms during a home visit and immediately notified us at the health facility. We met the client at his home and suggested he come with us to the health facility so we could test him. In this case, he tested positive.
This past meningitis season, a community health worker identified someone with symptoms during a home visit.
We immediately treated him and put him in isolation but our work wasn’t done. We had to do two things:
- Convince his friends and family not to visit him in the hospital.
- Talk to the community, especially religious leaders, about the disease and how it spreads.
In my town, if someone is ill and is in the health facility, family will often want to come to visit their sick kin. So we asked community health workers and trusted religious leaders to talk to this client’s family and help ensure they wouldn’t show up to visit him.
The community also needed to know why and how our client got sick, so we focused on wellness activities and taught people how to avoid the infection and the spread of the sickness. We also asked people to bury their deceased kin immediately, making sure no one touches the body at a funeral (a common custom before burial).
We know that these techniques work because the community listens. They trust us. They also see the danger they’re facing. When they see directly, the dangers of the disease, they really apply the measures we’ve asked of them. If we have cases that are particularly severe, we ask the Ministry of Health to help us launch a vaccination campaign.
Q: It sounds like your community trusts you. How did that relationship affect your town’s response to the COVID-19 pandemic?
I remember the day we received the first batch of the COVID-19 vaccine. It was June 2021, and our health facility received enough doses to vaccinate 400 people with the first dose. I gathered members of the community and religious leaders and sat down in a chair, ready to receive the first shot myself, in front of a group of people.
I did this because there were many myths and misconceptions about the vaccine, but I knew my community trusted me. If people saw me, a health worker, getting vaccinated it was a message to the community that the vaccine was good for them too. Three days later, all 400 doses had been administered.
There were many myths and misconceptions about the vaccine, but my community trusted me.
The lead up to this moment wasn’t easy though. People were either afraid of COVID-19 or skeptical. So we immediately started an information campaign, working with religious leaders and community health workers to inform the community about COVID-19, how it spread, and what the risks of infection were.
Once we taught them about these things, people were cautious. When they came in for health services, all of the measures advised by the health workers were respected. We used personal protective equipment and made sure there was enough ventilation in the health facility.
These steps helped our region be one of the least infected regions in Burkina Faso. People accepted information about COVID-19, adopted new daily routines, and got vaccinated.

Q: You have so much experience in pandemic prevention and response but that’s only part of your job. You spend most of your days responding to your clients’ everyday health needs. Can you talk about how that is interconnected? And does that help you with disease surveillance?
A few weeks ago, I was on night duty and a pregnant woman came in. She was spotting (light bleeding) and was achy all over. I checked her temperature and she had a fever. After my consultation with her, I conducted a rapid diagnostic test and she had malaria, a very serious diagnosis, especially for a pregnant woman.
Health facilities like mine are often the first point of contact between the community and the health system.
Health facilities like mine are often the first point of contact between the community and the health system. We receive many different types of sicknesses within our health facility and when the cases are severe, we refer them to the district level. But overall, we treat 90% of the cases that come into our facility. Our role within the community is to help members when they are suffering from illness, no matter what. Helping them feel safe, no matter what type of symptom. Encouraging people to come to the facility no matter what type of symptom.
I spend a lot of time in the community with my team, encouraging clients to come to the facility the minute they feel symptoms. I work very hard to make sure they understand the necessity to take charge of their own sickness. To encourage this, we provide free health services for children under 5 and pregnant woman. I’ve also made a point to learn the local language so I can speak to people in their mother tongue, rather than in French. With this strong connection to the community, we see at least 300 clients per week among our seven staff members at the facility.
In this case, I’m so glad the pregnant mother came in. We were able to treat her symptoms immediately. If she hadn’t come in when she felt symptoms, her baby’s life would have been in jeopardy.
At the UN General Assembly this week, Roger Zingue will be sharing his experiences with global health leaders to highlight four key messages about frontline health workers and their foundational role in pandemic prevention, preparedness, and response:
- They provide integrated care to treat people, not just diseases.
- They draw on trust to improve health in their communities.
- They need to be fully supported and integrated into health systems.
- They are the first line of prevention, preparedness, and response.
Katherine Seaton, communications manager, Jhpiego; and Chantelle Allen, senior technical advisor for primary health care, Jhpiego contributed to this article.
All photos by Souleymane Zare for Jhpiego.
