Health Workers in Many Kenyan Clinics Brave Community Health Care Alone
By Melissa Wanda, Family Care International, Kenya
In a village in rural Kenya, a woman in labor travels miles along rutted dirt roads to get to the nearest health center. She wants to give herself and her baby the greatest possible chance of surviving childbirth and returning home to begin new and healthy lives. When she arrives however, the gates are locked; the nurse has gone home.
Kenya, with only 11.8 health workers per 10,000 people (more than 40% below WHO’s recommendation of 22.8 per 10,000), is one of 57 countries — including 36 in Sub-Saharan Africa — with a critical shortage of health workers.
Many local health facilities have only one health worker, often a nurse, to provide all patient care. This puts a heavy strain on the health worker, and means that many intended 24-hour health facilities are often closed for extended periods of time. Kenya’s news media has also reported recent health worker strikes in reaction to late or non-payment of wages.
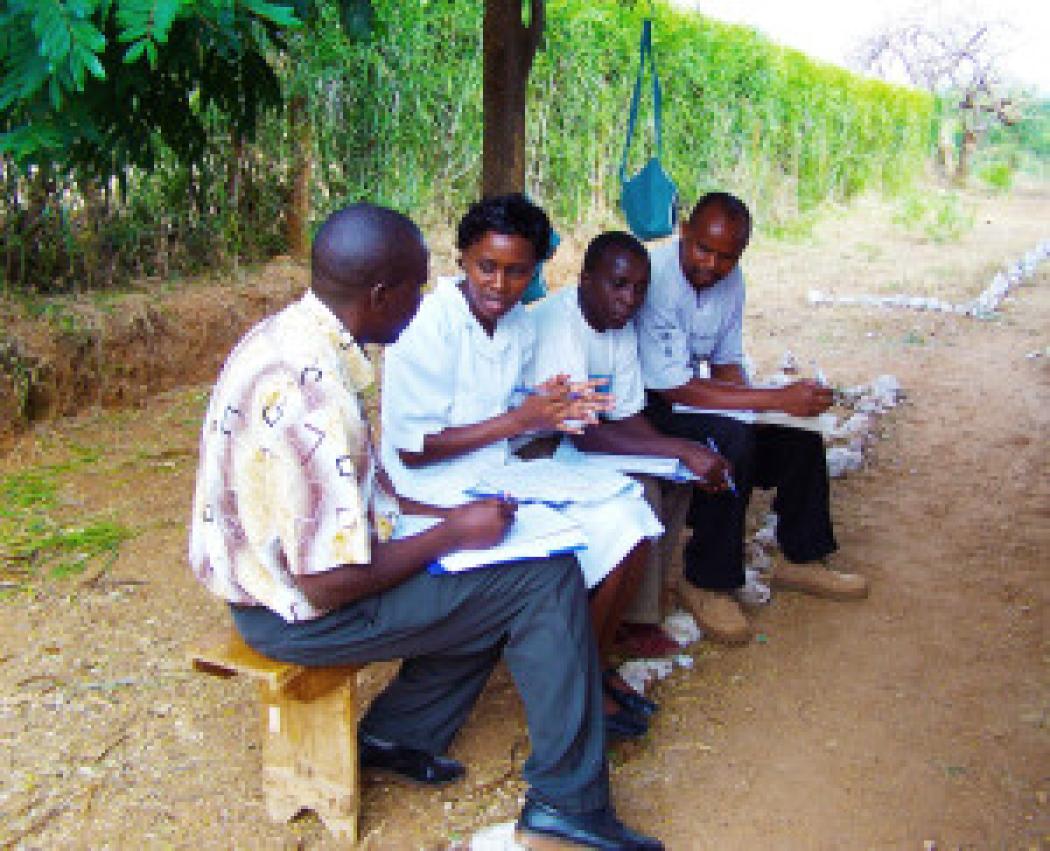
 Kenyan health workers share frustrations and challenges of working at understaffed health centers. Photo courtesy Family Care International.
Kenyan health workers share frustrations and challenges of working at understaffed health centers. Photo courtesy Family Care International.
The Government of Kenya has committed to strengthening human resources for health in the public health system. Several civil society organizations (CSOs) working to improve reproductive, maternal, newborn, and child health (RMNCH) have come together to advocate for the fulfillment of this urgently important promise. This alliance, co-led by Family Care International (FCI) and the African Women's Development and Communication Network (FEMNET) under FCI’s Mobilizing Advocates from Civil Society (MACS) project, is conducting advocacy at the county level in Kenya, since counties are responsible for making many health spending decisions in Kenya’s recently decentralized administrative structure and health system.
With support from the MACS project, Deutsche Stiftung Weltbevoelkerung (DSW), a member of the advocacy alliance in Kenya, has surveyed community perceptions of the need for more health workers, and explored how effectively county governments have invested in addressing those needs. Working in two urban and two rural counties, DSW conducted research at various levels of the health system, including outpatient dispensaries, health centers, and hospitals. DSW found that counties are not budgeting or investing spending adequately enough to ensure that facilities have enough health workers to provide high-quality services. Although special funding has been set aside nationally to hire new health workers, counties have mainly been spending this money to pay current staff. DSW is sharing these findings with MACS and county health authorities, leading to one county already committing to hire an additional 72 nurses.
DSW also brought together community members and health facility staff to discuss the state of care at local health facilities. Community members complained that lack of staff meant an absence of essential services, especially at night and on weekends. Health workers expressed the frustrations of working alone, often lacking the drugs and supplies they need to treat their patients, and the low morale that comes from working under those conditions. For example, one nurse described a recent evening when she was the lone nurse caring for six women in labor!
These community meetings opened new channels of communication, fostering greater understanding and accountability between health workers and the communities they serve. This enabled health system users and health workers to join together in search of practical solutions.
Peter Ngure, DSW’s project lead, shared with me a story about one community in which participants said they prefer to come to the hospital — a long distance from their homes —in the afternoon, so they have time in the morning to travel there. In response, the hospital rearranged staff work schedules, deploying more nurses in the afternoon than morning hours. Similarly, community members learned that the hospital holds Monday afternoon staff meetings, helping to explain why appointments are often unavailable at that time, which had been a repeated source of frustration and confusion.
“This dialogue between community members and health workers helped to build much-needed goodwill during these very challenging times,” said Mr. Ngure.
FCI, DSW and the members of the civil society advocacy alliance will use these findings and experiences to hold county governments accountable for addressing the health worker shortage. When the Kenyan Ministry of Health releases its upcoming human resources for health strategy, which will provide specific guidance on exactly how many health workers should be assigned to each health facility, alliance members will work to make sure that counties follow that national policy, so that every Kenyan mother, seeking care for herself and her baby, will be greeted by open gates and a health worker with the skills and resources to ensure their survival and good health.
